Signs and symptoms of depression
If low mood is having an impact on your life, you might be wondering whether you’re experiencing depression. Find out more about the signs and symptoms, along with commonly related health issues.
Depression is a common mental health condition that can influence the way you think, feel and function.
It doesn’t always look the same from person-to-person. For some, it shows up as persistent sadness or hopelessness; for others, it may appear as fatigue, numbness, irritability, or a loss of interest in the things that once mattered. These changes can develop slowly or happen suddenly, making them difficult to recognise at first.
Join our expert psychiatrist, Priory's Dr Victoria Chamorro, as she breaks down the core, physical, behavioural and often missed symptoms of depression.
Depression can affect every part of a person’s life, not just emotionally, but physically and socially too. The symptoms can vary widely from one person to another.
Below are symptoms of how you might feel if you’re struggling with depression and how your body might react to the depression.
Depression can also influence how you interact with others and how you manage your daily responsibilities. You may start to notice shifts in your habits, motivation or ability to cope.
Common behavioural and social symptoms include:
These changes can feed into feelings of isolation, guilt or low self-worth, creating a cycle that can be hard to break without support.

Depression can deeply affect how you think and feel. You may find yourself overwhelmed by negative thoughts, or unable to connect with the world in the way you normally would.
Common psychological symptoms include:
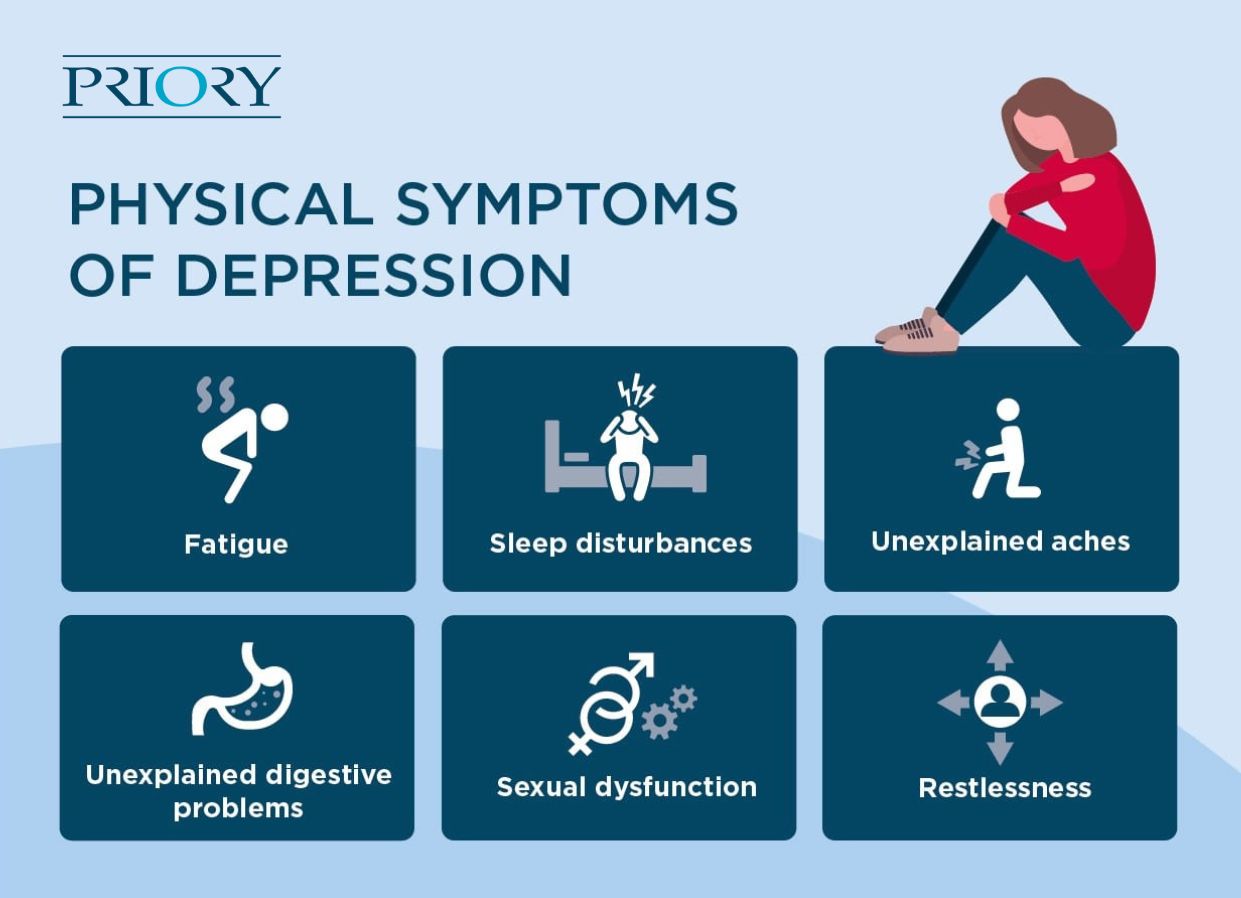
Depression can have a significant impact on your body, affecting longer-term physical health. Sometimes, these physical symptoms are the first signs people notice.
Common physical symptoms include:
It’s common for these physical effects to be mistaken for other health issues or dismissed entirely, which can delay getting the right support.
Depression doesn’t look or feel the same for everyone. For some people, the signs build slowly over time. For others, symptoms appear more suddenly or may be triggered in response to a life event.
Depression is often described in terms of severity, but it isn’t about how bad it looks from the outside. It’s about the impact that your symptoms are having on your relationship with yourself, your overall wellbeing and your quality of life.
There are different types of depression to be aware of, and even mild symptoms deserve attention. You don’t need to wait until things get worse before seeking help.
There’s no one way depression starts. Sometimes the signs are obvious; other times, they can creep in gradually and be harder to spot.
Symptoms may develop over time, making it difficult to recognise there’s a problem at first. They may also follow a specific event, like a bereavement, illness or major life change. For some, depression symptoms may occur in episodes. Whether you have single, recurrent, or seasonal symptoms – such as in seasonal affective disorder (SAD), you deserve to get the support you need.
If you're unsure whether what you're feeling is depression, tools like questionnaires or symptom checklists can be a helpful first step. These are often used by GPs or mental health professionals to understand what you're experiencing and help you move forward.
You can try a quick, confidential depression self-assessment to see how your symptoms compare.
Low mood, tiredness, or feeling emotionally flat can have many causes. While a qualified professional can help with a diagnosis, you can start to make sense of what you’re feeling by understanding the differences between depression and other conditions.
Here are a few common experiences that can overlap with depression:
Grief, which can trigger sadness, withdrawal and exhaustion. While grief can look and feel like depression, it tends to come in waves and eases with time. Depression, by contrast, often brings a persistent sense of hopelessness and worthlessness, with regular self-critical thoughts or suicidal feelings
Burnout, which is a state of emotional, physical and mental exhaustion caused by prolonged stress. It’s often situational and might be related to work, caregiving or feeling overwhelmed by responsibilities. It can lead to low motivation and concentration, similar to depression, but tends to improve with rest and lifestyle changes
Hormonal changes, or mood changes linked to hormone fluctuations, can also mimic depression. They might be connected to the menstrual cycle, menopause, postnatal changes, thyroid issues or premenstrual dysphoric disorder (PMDD). These shifts can affect sleep, energy and emotional stability, and are worth discussing with your GP
Seasonal changes, which can cause your mood to dip during certain times of year. This most commonly occurs for people in winter, which could be a form of depression known as SAD. This can involve tiredness, low motivation and a change in appetite.
Depression can affect anyone, but symptoms may look different depending on age, gender or life stage.
If you’re experiencing symptoms of depression that are starting to affect your daily life, remember that help is always available. You don’t have to wait until things feel overwhelming to reach out.
You might want to speak to a GP or mental health professional if:
Support is available through NHS services (through your GP or by self-referral in England), private therapy or psychiatry, mental health helplines and support services. If you’d like to explore options for professional support, you can learn more about depression diagnosis. You can also try our confidential depression self-assessment to better understand what you’re experiencing – whether you’re just starting to explore symptoms or looking to take the next step.
If depression is diagnosed, your care plan might include:
You’ll receive support that’s personalised to you, whether through inpatient, day care or outpatient treatment.